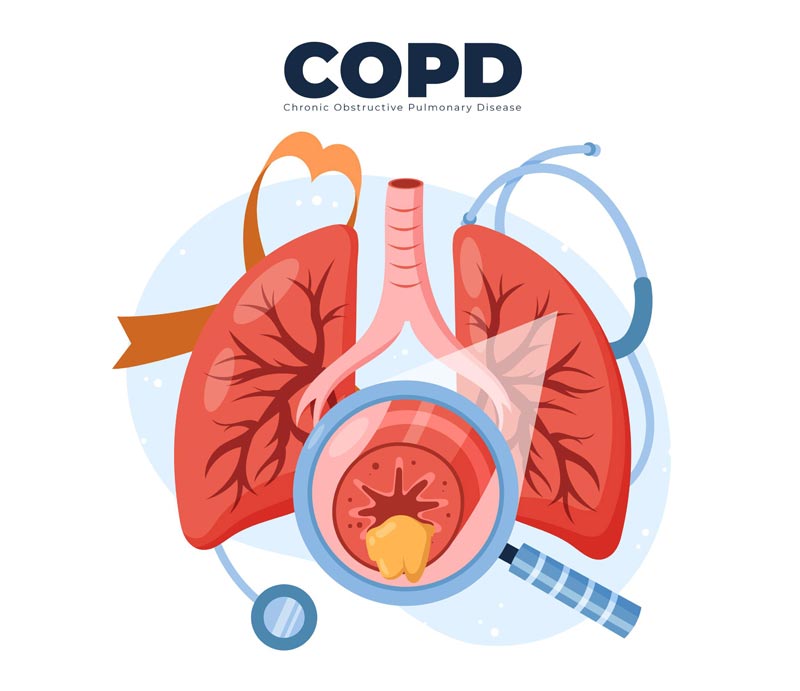
COPD –
Chronic Obstructive Pulmonary Disease

What if your lungs were being destroyed slowly, and you had no clue?
Chronic obstructive pulmonary disease or COPD is one of the leading causes of non-communicable disease deaths globally and is the second most common cause in India.
A neglected chronic lung disease, COPD is a silent killer that can easily be managed with appropriate treatment.
Chronic obstructive pulmonary disease or COPD is an incurable group of progressive lung conditions. The most common of these diseases are emphysema and chronic bronchitis. As many people with COPD have both these conditions, it is important to focus on lung health and understand how to manage COPD.
The air that we breathe travels from the nose and windpipe to the bronchi – the two tubes leading to the lungs. From the bronchi, the air travels to smaller tubes in the lungs that branch out like a tree. At the end of the tubes, there are small air sacs made of fragile tissues. These sacs help oxygen to be absorbed in the bloodstream and transfer the carbon dioxide to be exhaled out of the body.
With COPD the airways in your lungs are affected. They become inflamed, causing airflow obstruction. The tissue or air sacs that absorb oxygen are destroyed, making it harder to get rid of the carbon dioxide. As the disease progresses, the patient can experience shortness of breathing and wheezing.
The COPD symptoms are mild to begin with. People may confuse it with the common cold. Intermittent coughing, shortness of breath after certain activities like exercising or climbing the stairs may be the first signs of COPD. Do not ignore it or blame it on ageing. If you experience these symptoms or think are at risk of developing COPD, it is always better to consult a specialist.
A few early signs of COPD
These symptoms can get worse because of smoking or being exposed to secondhand smoking. Long-term exposure to irritants or air pollution too can affect the situation. If you find yourself avoiding physical activities, it could be because of COPD. It is important to be vigilant about the early symptoms, as ignoring it will worsen the issue. Early detection is key to successful treatment of COPD and overall disease management.
COPD Symptoms at later stages:
As the situation worsens, the patient will experience breathlessness, chronic cough, frequent respiratory infections, producing excessive mucus or phlegm. In extreme cases, the fingernail beds and lips could turn blue because of lack of oxygen. A person might feel confused or disoriented and experience extreme fatigue.
Smoking is the most common cause of COPD. COPD develops over several years as your lungs are increasingly damaged. However, it rarely becomes noticeable until after the age of 40. Damage of lungs is directly proportional to the exposure to active or passive smoke. Apart from smoke, people can develop COPD from being exposed to biomass, micronized dust particles and air pollution from industrial chemicals. This includes being exposed to second-hand smoke for long periods. There is an inherited condition called alpha1-antitrypsin deficiency, which causes COPD in some people.
The symptoms may seem minor at first but can progress to the point where daily activities such as walking, getting dressed, and even eating can cause extreme shortness of breath. COPD can be mild, moderate or severe depending on the extent of lung damage.
If you see these symptoms in yourself or a loved one, make an appointment. Acting early is essential to take control of the disease so you can live better with it.
A medical professional will evaluate your symptoms and understand the family history. Based on the initial examination, the doctor might recommend a few tests. One of the most reliable tests for detecting COPD is spirometry.
In spirometry, a person blows out long and hard into a tube attached to a machine, which measures the time it takes to empty your lungs. The more obstructed your airways, the longer it takes to blow the air out. Spirometry tests are available in most areas either at public hospitals free of charge, or at larger medical centers or private laboratories where a charge may apply. Spirometry can detect COPD before symptoms develop.
Spirometry is a cheap, simple and reliable method for the early detection and monitoring of COPD patients, and for establishing a differential diagnosis. Spirometry gives immediate results and communicating the results to smokers has shown to motivate them to quit. Your doctor also might use the test results to find out how severe your COPD is and to help set your treatment goals.
Oxygen Saturation Test:
Oximetry helps in estimating the amount of oxygen in the blood stream. The oxygen saturation level can be an indicator of lung health.
Apart from these, depending on the condition, the doctor might ask for a chest X-ray, ECG, blood test, CT scan, peak flow test, etc.
Chronic Bronchitis:
This is a chronic obstructive airway disease that affects the airway linings of the lungs. In chronic bronchitis, the airways are inflamed and narrowed and the hair like fiber called cilia that line the bronchial tubes vanish. These fibers help move the mucus out. When the airways swell, it causes shortness of breath and coughing. This makes it difficult for your lungs to inhale and exhale air. Losing cilia makes it difficult to cough out the mucus from the lungs. If you have had a persistent cough, shortness of breath and mucus for over 3 months in two different years, then you might be suffering from Chronic Bronchitis.
Emphysema
Emphysema is a condition that affects the air sacs (alveoli) of the lungs. It directly affects the way your lungs transfer oxygen into the bloodstream. Emphysema damages the walls inside the air sac, resulting in poor absorption of oxygen in your blood. If untreated, then the lungs may lose their elasticity permanently, causing air to be trapped into the lungs.

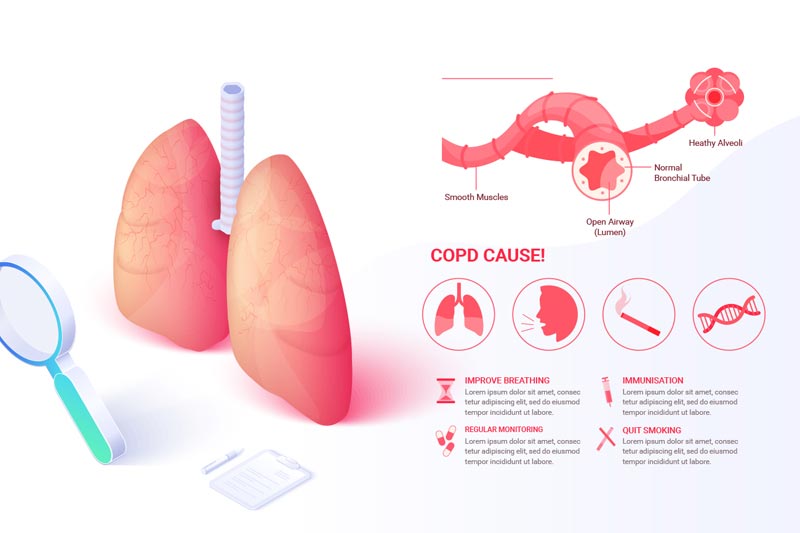
The first and most crucial treatment of COPD in smokers is to quit smoking. Medications and other therapies are available to help treat nicotine addiction and quit smoking. Medications can also be prescribed to help relieve symptoms of COPD and to prevent symptom flares (called exacerbations) that can lead to further loss of lung function. Some general classes of medications include those that aim to widen the airways (bronchodilators), decrease swelling in the airways (anti-inflammatory drugs, such as corticosteroids), and/or treat infections (antibiotics). Other than antibiotics, most COPD medications should be taken every day, usually for life. In some people, COPD can also cause the oxygen level in the blood to be low. If this occurs, a person may be given supplemental oxygen. Breathlessness should not be confused with low oxygen levels. People with COPD can experience shortness of breath or have a hard time breathing, even if they have good oxygen levels.
The term chronic, in chronic obstructive pulmonary disease, means that it lasts for a long time. Symptoms of COPD sometimes improve when a person stops smoking, takes medication regularly, and/or attends pulmonary rehabilitation. However, the lungs are still damaged and can never fully return to normal. Therefore, COPD is a lifelong condition. Breathlessness and fatigue may never go away entirely, but people can learn to manage their condition and continue to lead a fulfilling life.
Acute exacerbation or COPD flare-up. is a sudden worsening of COPD symptoms compared to the usual severity of symptoms. This often means a worsening of breathlessness and an increase in coughing, with more phlegm (sputum)
Acute flare-ups (exacerbations) of COPD occur more often if your COPD isn't well controlled and you have more severe ongoing symptoms.
Upper respiratory tract infections or chest infections caused by viruses or bacteria or physical exercises cause most exacerbations.
Terrible air pollution can also cause exacerbations, especially in big cities.
When you see a healthcare professional, they might notice that:
The general principles of treatment are to increase the inhalers that open up the airways (bronchodilators) and to take an oral steroid (usually prednisolone). Antibiotics should only be used if there is any evidence of a bacterial infection.
You should act quickly as soon as you realise that your symptoms are getting worse. Most people with COPD are given a treatment plan to follow if the symptoms get any worse. This often includes having a supply of steroid tablets (prednisolone) to start as soon as any increased breathlessness affects your activities. They will also often give you an antibiotic to take as soon as your phlegm (sputum) changes colour.
However, it's very important to see your doctor if your symptoms don't get better quickly or if your symptoms are really bad or if you have any concerns.

If your symptoms are very severe, or if treatments at home are not working well enough, you may need to be admitted to hospital.
If you are very breathless, it may be impossible to use your inhaler. Nebulisers are machines that turn the bronchodilator medicines into a fine mist, like an aerosol. You breathe this in with a face mask or a mouthpiece.
Although nebulisers are usually no more effective than normal inhalers used with a spacer device, they are useful if you are exhausted with the increased effort of breathing.
You may need oxygen to help you breathe. Sometimes a special machine (either a bi-level positive airway pressure (BiPAP) machine or a continuous positive airway pressure (CPAP) machine) is used to help you breathe.
This is called non-invasive ventilation (NIV). It consists of a close-fitting facemask and drives oxygen into your lungs, forcing the airways to open.
In very severe cases, you might need more help with breathing in an intensive care unit (ICU). A tube may be put into your windpipe and connected to a machine that 'breathes' for you (a ventilator).
It is really important to reduce your risk of having any further flare-ups (exacerbations) as they make you unwell and frequent exacerbations may worsen your usual symptoms, even when you are not having an exacerbation.
The risk of having any further exacerbations can be reduced by:
As COPD affects the health of your lungs, it can have long term adverse effects like respiratory infections, lung cancer, high blood pressure and heart problems. It is important to manage the disease with a good treatment plan and lifestyle changes. Good management can make living with the chronic disease comfortable.
© 2026 Healthy Lungs.