What is
Allergic Rhinitis?
Do you fear season change as it causes frequent sneezing, sore throat and cold?
Are you allergic to dust, pollen or similar?
If the answer is yes, then you are mostly suffering from Allergic rhinitis
According to the American Academy of Allergy, Asthma and Immunology, approximately 10-30% of people suffer from allergic rhinitis worldwide. Tree pollen, ragweed, animal dander, dust and mold are some of the common allergens that cause allergic rhinitis and are most common in the age group of 20-40.
Allergic symptoms are miserable and usually affect the quality of life, but they can be managed effectively with the help of medication and lifestyle modifications.

Allergic Rhinitis is a type of inflammation in the nose, caused by the overreaction of the immune system to the allergens.
Some people suffer from allergic symptoms, when the season changes (like at the beginning of spring or fall season), while others suffer from allergic symptoms all year round.
Signs and symptoms of allergic rhinitis can differ from person to person. They can range from mild to moderate and may cause complications of allergic rhinitis at a later stage.
Some of the common symptoms of allergic symptoms are:
Seasonal Allergic Rhinitis:
As the name suggests, seasonal allergic rhinitis occurs during the change of season, usually in the spring, summer and early fall seasons. Environmental factors like tree, grass and ragweed pollen are common allergens that cause seasonal allergic rhinitis.
Perennial allergic rhinitis:
This type of allergic rhinitis occurs all year-round. Indoor allergens like pet dander, dust, mold, etc. can be a primary cause of perennial allergic rhinitis and the symptoms persist irrespective of the season.
Occupational allergic rhinitis:
This is another common type of allergic rhinitis caused by work-related exposure to certain chemicals or irritants.
Genetic factor:
Although allergies can affect anyone, having a family history of allergies increases the chance of developing allergic rhinitis, making you more susceptible to it. A family or personal history of other allergic disorders like asthma, atopic dermatitis also increases the risk of developing allergic rhinitis symptoms.

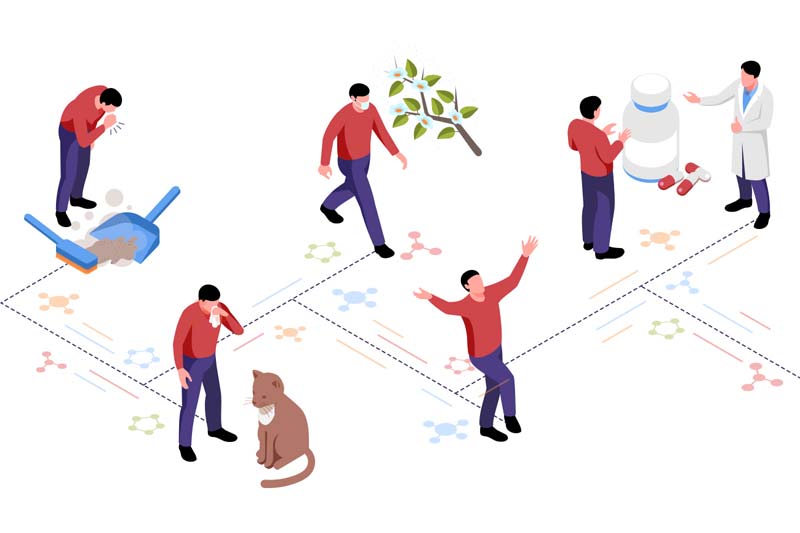
Environmental factor:
These are some common environmental factors (external allergens) that increase the risk of developing allergic rhinitis.

These allergens (like animal dander, tree pollen) remain harmless and do not cause any symptoms in most people. However, in sensitive individuals, these allergens cause overreaction in the immune system, leading to allergic rhinitis symptoms.
When sensitive individuals inhale these irritants or allergens through the nose or mouth, their body defends and releases the inflammatory chemical histamine from mast cells as a defensive mechanism. Releasing histamine from mast cells causes the development of common allergic rhinitis symptoms.
Most often, the diagnosis is made by your healthcare provider based on a full health history and physical examination. Besides the above signs, the healthcare provider may find:

Your doctor may also perform a skin allergy test and a blood test to determine your allergy triggers.
Skin prick allergy test:
In this test, few different allergens are inserted into the skin. Doctor records, analyzes and reviews the individual allergic reaction caused by different allergens.
Blood Test
A blood test to check the immunoglobulin E (IgE) antibody is another useful diagnostic test that helps in confirming allergic rhinitis diagnosis. This test measures the level of IgE antibodies in the blood and helps in the detection of allergies to a particular substance.
A complete blood count test (CBC) helps diagnose allergic rhinitis. People with allergies usually have an elevated eosinophil count.

The treatment of allergic rhinitis involves the use of various medications that include pills, nasal spray and allergy shots.
Here are some common effective medications for allergic rhinitis:
Antihistamines:
Antihistamines are the most commonly used medication for treating allergic rhinitis symptoms. They work by blocking the action of histamines and help in controlling allergic symptoms. Although antihistamine medication is available as over-the-counter medication, some of these may cause side effects like sleepiness and drowsiness. It could also interfere with other medications or existing health conditions, hence talk to your doctor before starting any medications. Cetirizine, levocetirizine and fexofenadine are some of the commonly used antihistamine medications.
Decongestants:
Decongestants help reduce the symptoms of nasal congestion. Decongestants are available as tablets, syrups, drops and sprays, however long-term use may cause other side effects. Some decongestants may increase blood pressure. It is best to take professional advice before using them. Pseudoephedrine and phenylephrine are some commonly used decongestants.
Corticosteroids Nasal sprays:
Corticosteroids nasal sprays are effective medication for allergic rhinitis. They help in reducing nasal congestion and relieve allergic symptoms. They are recommended to be used for the long term; for better control of allergy symptoms.
Leukotriene inhibitors:
Leukotriene is a type of chemical that the body releases as a defensive mechanism when exposed to allergens. Leukotriene inhibitors help to block the leukotriene secretion and control allergic symptoms.
Immunotherapy (allergy shots):
Immunotherapy is used for severe cases of allergic rhinitis. In this therapy, allergy shots are used to decrease your immune response to a particular allergen. This is a long-term treatment plan. In each setting, the doctor increases the dose of allergens and helps you in developing immunity against particular allergens. This is a long-term treatment plan and requires commitment from patients.
When left untreated, allergic rhinitis can cause complications.
Allergic rhinitis is not a life-threatening condition. Though allergic symptoms are miserable and affect the quality of life negatively, medication and lifestyle modification can help manage them effectively.
© 2026 Healthy Lungs.